72 years old female came with c/o SOB since 3 days , fever and cough since 3 days.
Hi, I am Y.Shasshank , 5th semester medical student.
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed throughout the piece of work whatsoever.
Chief complaint:
Patient with c/o SOB since 3 days c/o fever and cough since 3 days
History of present illness:
Patient was apparently asymptomatic 3 days ago the she developed SOB which is grade 3, gradually progressive. No c/o orthopnea/PND.
Fever since 3 days low grade ,continous, not associated with chills and rigor.
Cough is productive with white colored sputum, non blood tinged
No h/o chest pain,palpitation
No abdominal pain,vomiting, loose stools
Past history:
K/c/o Hypertension, Diabetes mellitus type 2 since 2 years.
N/k/c/o asthma,epilepsy,TB,CAD,CVA.
Treatment history:
Drugs used for Diabetes and Hypertension.
Personal history:
Married
Mixed diet
Normal appetite
Irregular bladder movements - increased in frequency and burning micturition
Regular bowel movements
No allergies
No addictions
Family history:
No significant Family history
General examination:
Patient is conscious,coherent and coperative.
Well built , moderately nourished and well oriented to time,place and person.
No Pallor
No Icterus
No Cyanosis
No Clubbing of fingers
No Lymadenopathy
No Pedal edema
Vitals:
Temperature: 101°C
PR: 97 bpm
RR:22 cpm
BP:140/90 mm Hg
SpO2: 83%
GRBS: 174mg%
Systemic examination:
CVS - S1, S2 heard
CNS - Higher motor functions intact
PA - Soft and non tender
RS - BAE+ , NVBS +
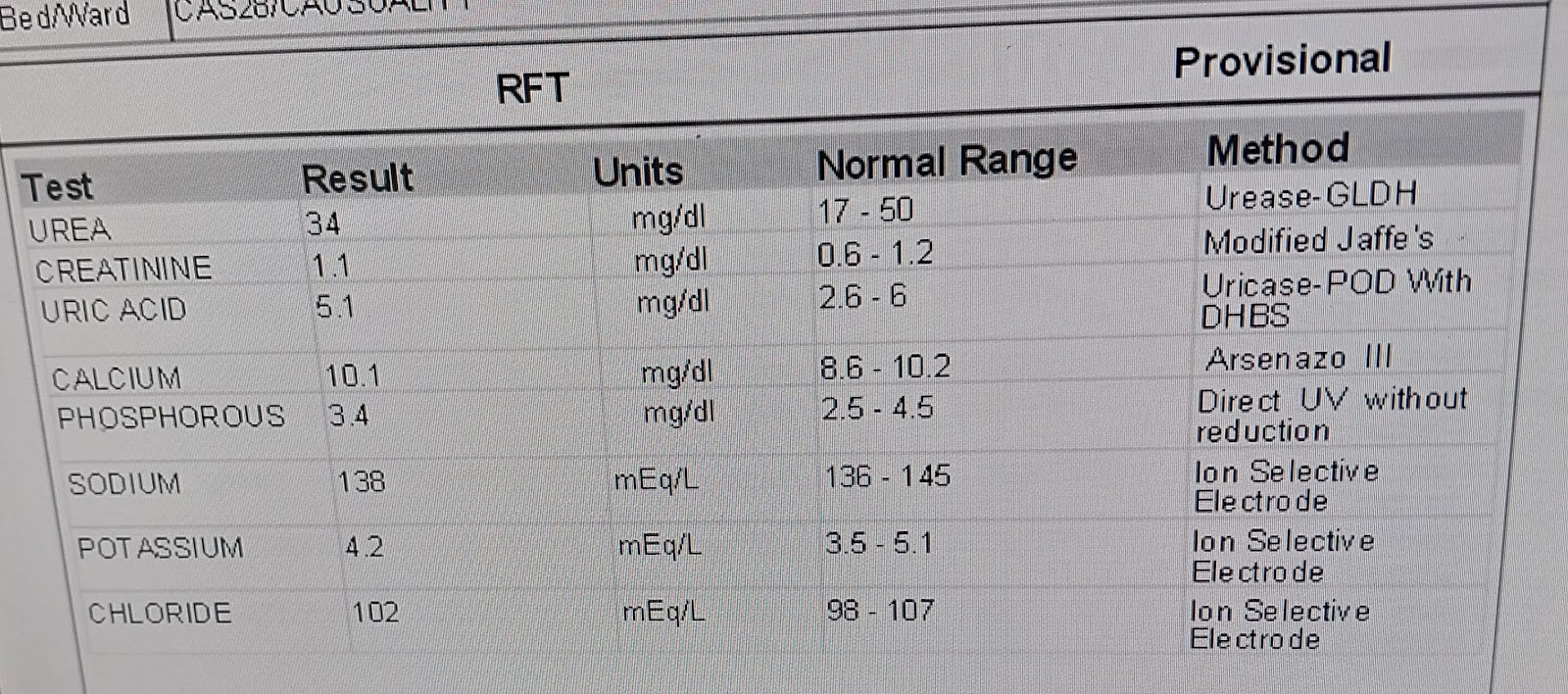
Investigations:



Comments
Post a Comment